Death represents a significant and vulnerable point in time for all when a love one is facing daeth. While everyone would prefer to focus on life, a significant amount of stress related to death can be reduced by proper planning. Here’s some guidance on how to ensure optimal end-of-life care for all involved.
1. Know the options: What’s the difference between hospice and palliative care?
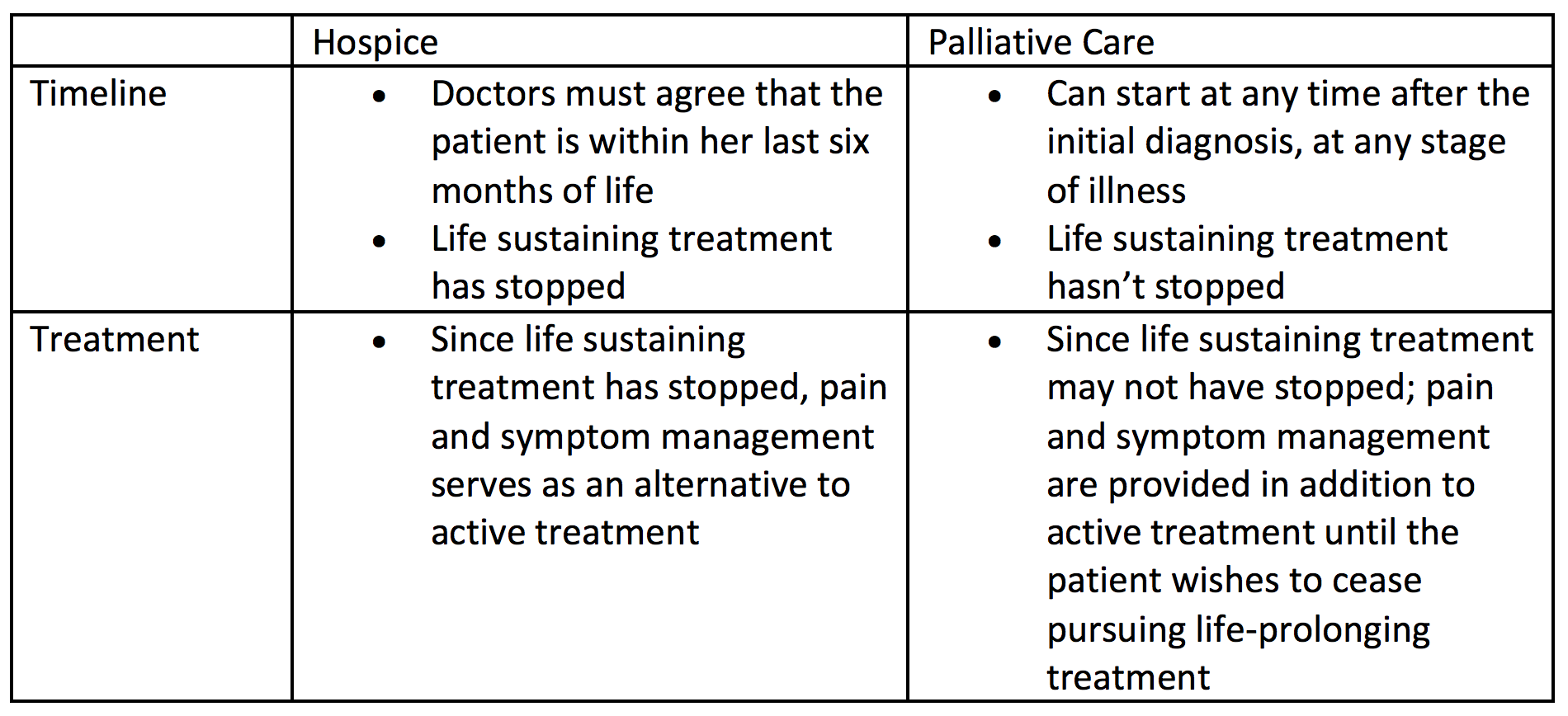
Both hospice and palliative care provide end-of-life care, including pain and symptom management and comfort for the loved one while he prepares for death. Both offer end-of-life care in the home or in a facility with a team of specialists who deliver this care. However, there are a few differences:
2. Dot your i’s and cross your t’s: Are all the necessary legal documents in order?
While competent, the loved one should express her wishes to help guide family members when she can’t make decisions for herself. This includes: directions as to what type of care she wants; whether she would like to donate organs (and when that should be communicated to medical professionals); preferred end-of-life care (hospice or palliative care); and the location. This can be included in a healthcare care directive/proxy or in a separate letter to the family, but it should be done with a higher level of formality, such as the help of an attorney, to communicate the legitimacy of the loved one’s wishes.
- Health care directive/proxy: In this document, the loved one will appoint a surrogate decision-maker or proxy to make medical decisions for her once she’s no longer considered able to make competent decisions and provide informed consent. Without this in place, family members won’t be able to make medical or care decisions for their loved one; they’ll have to go through the courts to attain permission. This process can be time-consuming and expensive, detracting from the care of the love one.
- Living will: This document tells family members and surrogate decision-makers whether the loved one would like to receive additional measures of care. This includes instructions for extraordinary measures, such as respirators, resuscitation, antibiotics, and withholding or withdrawing life-sustaining treatment. This document is also a good place for the patient to instruct whether she would like her organs donated after her death.
- Health Insurance Portability & Accountability Act: This document protects the privacy of the patient’s medical records and other information. This is especially important if the loved one is unable to make decisions, allowing family members to get second opinions and to transfer her between facilities.
3. Broach the subject: Has there been a discussion with the loved one to understand what her wishes are?
Ultimately, the loved one should be in control of her death, and family members should know what that means for her. When the time comes when she’s no longer mentally competent to make her own decisions, her surrogate decision-maker will step in to be her voice. It’s important for the surrogate decision-maker to keep in mind the loved one’s wishes. This is by no means an easy conversation but can help bring peace of mind to the loved one in knowing what a good death means to her.
4. Nail down the timeline: When does the loved one want end-of-life care to begin?
Studies have found that there are many people who put off end-of-life care. This is often because the loved one is still fighting his illness and doesn’t want to receive end-of-life care until he’s done receiving preventative treatment. This can minimize the benefits of end-of-life care, as he has less time to prepare for death. To be eligible for hospice care, patients must be within their last six months of life. If the loved one isn’t yet done fighting his illness, hospice may not be the right decision. If he wants to continue receiving preventative treatment, palliative care may be the better option. It’s important to note that when hospice care starts, the loved one will no longer see his regular doctors and will only be under the care of the hospice staff. However, if a new treatment becomes available while the loved one is receiving hospice care, he can leave hospice to receive life-prolonging treatment.
5. Research reputation: Has the family discovered all information about the potential care facilities being considered?
Not all facilities offer the same benefits. Look at the reputation of each facility, and ask for references and look up reviews and any news online. Also, make sure they provide quality care and don’t have a history of promising services not delivered, and find answers to questions like, Do they have a history of withholding pain medication from patients due to fear of addiction? Do they have a history of ethical or staff issues? In addition, find out the last time the facility was inspected by the state or federal government, which may reveal if there were any issues. If there were, check how they were resolved.
6. Find out who’s behind the mask: How well does the family know the loved one’s care providers?
Communication is a key factor. Few medical professionals have explicit training in death and dying. So, to start, develop a good relationship with the loved one’s doctors to help understand the process; it will make the loved one feel more comfortable. And learning the communication habits between the doctor and the other professionals is extremely important. And make sure that any staff coming or going knows the protocol and why. As mentioned above, reports of staff withholding pain medication when the goal of end-of-life care is to provide comfort and free of pain has become a major concern. Finally, some facilities use outside and volunteer services who interact with patients and their families, so learning what screening and training they have had can bring peace of mind.
7. Do due diligence: Has the family done their own research? Have all factors that could influence their decision been explored?
Not all facilities are created equal. Hospice and palliative care have facilities across the nation; however, their standards vary. Ask the facilities being considered for references and if anyone has been in a similar situation, and if so, ask her how she was treated by that particular staff and if they followed through with their promises. Also, ask care providers to share some good methods that can be done by the patient’s loved ones to help. Most of all, check that each care provider is well-informed on the ethical issues in this area of care.
8. Learn the ins and outs: Is in-patient or out-patient care best for the loved one and family?
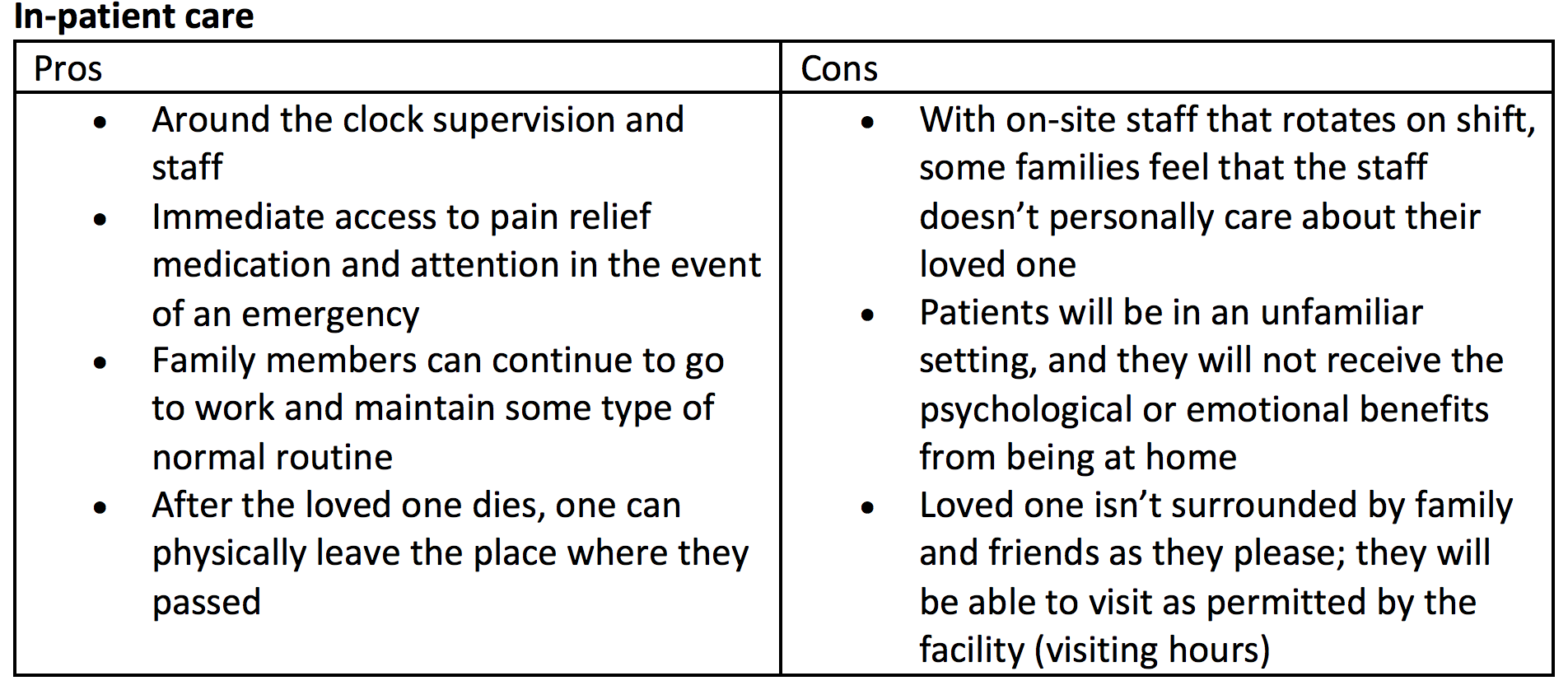
The physical location for end-of-life care is a significant decision for the loved one. It’s important that she feels comfortable in her environment during the final days of her life. Unfortunately, this isn’t always possible to achieve, since some families may not be physically equipped to care for their loved ones at home (out-patient care) and some aren’t financially able to allow their loved ones to stay in a facility (in-patient care).

9. Prepare Plan B: Does the family have a backup plan?
This may be most important for those who have decided to use out-patient care. Despite what promises are made by the end-of-life care provider, families should always have a backup plan. Recently, stories in the media have drawn attention to negative hospice and palliative care experiences. The reasons have ranged from poor communication to organizations not delivering on their promises. A common complaint is that staff doesn’t treat patients who are in pain as time-sensitive, and the loved one’s doctors and nurses were unreachable. For situations such as these, it’s important to have an alternative.
One option that many have found helpful is to have a comfort kit, which includes two pain relievers that can be administered to the loved one, should he be in pain when help is unable to come in a timely manner. One should ask for a comfort kit from the loved one’s care providers and shown how to properly administer the medication to the loved one.
10. Ask for help: Could the loved one and her family benefit from counseling?
Death is a highly stressful process for the person who’s dying and for her friends and family. It’s extremely important for all parties to feel informed about what they’re undergoing. The loved one should be able to reach a point of finitude, coming to grips with eventual death—this is a long process that can occur on many levels. On a surface level, this can begin with preparing any necessary legal documents and, on a deeper level, can include reminiscing, enjoying positive moments, saying goodbyes, passing on sentimental items or of significance and validating her life how she sees fit. This shouldn’t solely be left for the loved one to realize on her own. When faced with a terminal diagnosis and death, people have many different reactions. It’s important to offer the loved one guidance during this time. This will allow the loved one to have a death filled with control, dignity, peace and finitude.
This process has an end for the loved one while the family members must return their lives. Rituals after death such as religious traditions, a funeral and/or memorial service can be helpful, serving as a distraction and allows time to celebrate the loved one. However, at the end of this period, family members will no longer have any distraction from their grief and may need guidance. It’s important for those left behind to understand the different stages of grief they may be experiencing, and healthy coping techniques that may help them.





